
A hospital serves patients best when it combines advanced resources with simpler components of recovery. Medical miracles can make it easy to forget time-honored curative factors like air, daylight, common-sense pathogen control, and comfort.
Stephen Yablon, AIA, designer of award-winning healthcare spaces around New York, begins from the patient’s perspective. “What’s disorienting and frightening about being sick is you’re removed from your friends—from your life,” he observes. “So any feeling that can reinforce a connection to life outside or nature is healing.” Knowledge of environmental effects on health, he continues, extends from ancient Greece to “the early days of the modern movement, where architects like Alvar Aalto and Berthold Lubetkin saw a strong correlation between the quality of design and the quality of care.”
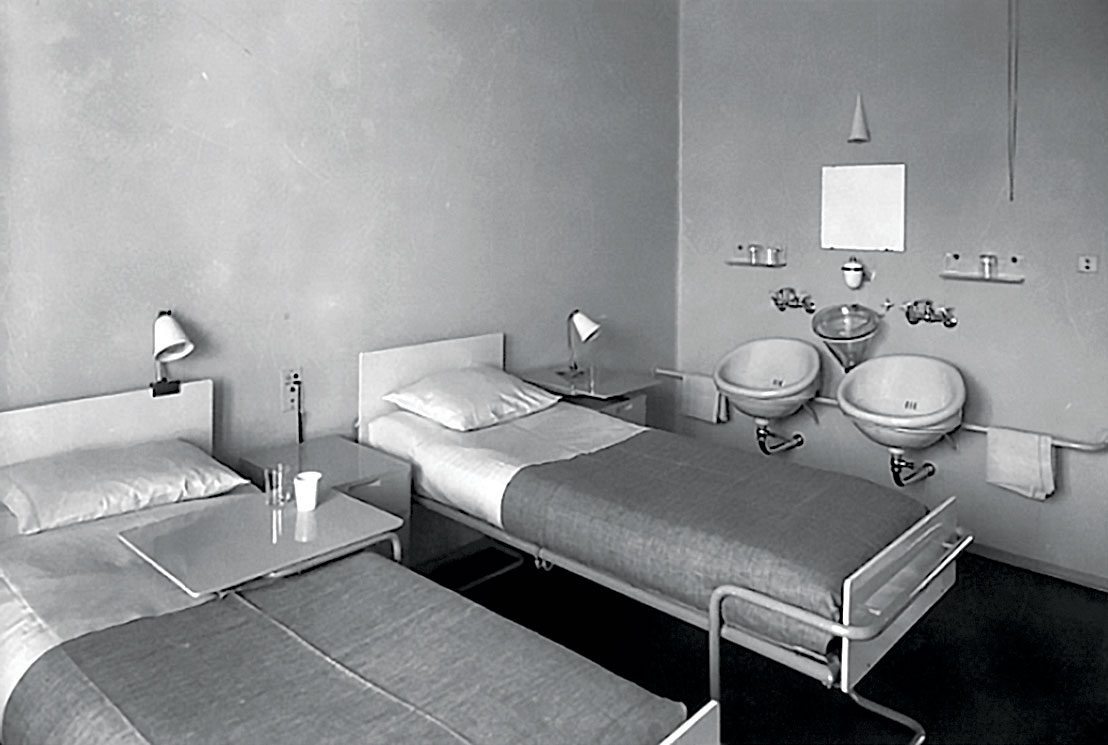
In the mid-20th century, however, with the advent of exponential advancements in healthcare, the patients’ subjective considerations were not seen as important anymore. As medicine grew more industrial, modernism abandoned the social ideals expressed in Aalto’s Paimio Sanatorium Preitila in Finland and Lubetkin’s Finsbury Health Centre in London.
Dehumanizing environments in today’s U.S. healthcare system are familiar. A patient endures kludgy Frankenbuildings: cramped, disorganized waiting areas; unnavigable, equipment-strewn corridors; inpatient rooms lacking stimulation and dignity; and half-hearted aestheticizing gestures, all in an atmosphere of stale air, eerie fluorescent light, and noise that makes sleep impossible. The healthcare setting is often the polar opposite of a healing space.
Recognizing these problems, progressive architects are designing spaces that promote both advanced interventions and natural processes. The field of evidence-based design (EBD) is using architecture, medicine, and public health to back up intuitions about nature’s effects on patient healing. (A 1984 study, for example, found that patients recovering from gallbladder surgery had shorter hospitals stays and needed less pain medication if their hospital windows faced a natural setting rather than a wall or parking lot.)

Yablon cites Maggie’s Centres for palliative care in the U.K and Hong Kong among the most influential architectural achievements in recent years. “They have the attitude that healthcare architecture does not have to be unchallenging,” he says; their design “makes you feel connected to life.” Still, ambulatory and inpatient spaces are not homes, and clients don’t want them too homelike. “You want a building to communicate that you’re getting the latest in care,” says Yablon. Today’s healthcare design aims to strike a balance between state-of-the-art expertise and personalized care through natural materials and lighting, patient-friendly circulation, and details that promote patient activity.
SOMETHING IN THE AIR
Patients want to have an active role in their recovery. “The ability to control one’s own environment is oddly not as common as you might think in hospitals,” says William Roger, FAIA, regional leader of healthcare practice at HOK’s San Francisco office. For inpatients, autonomy can involve something as simple as an operable window.
In two exemplary Singapore hospitals, Roger’s HOK colleague Mara Baum, AIA, told a recent AIA National Conference audience, “Form follows performance.” That nation’s medical system outperforms the rest of the world on efficiency metrics including life expectancy and cost, according to Bloomberg rankings. (The U.S. comes in 44th of 51.) Despite the hot, muggy climate, HOK’s Ng Teng Fong General Hospital (NTFGH, a 2017 AIA COTE Top Ten award winner) and RMJM’s Khoo Teck Puat Hospital achieve impressive results by EBD criteria: natural ventilation, passive cooling, and ample vegetation in patient spaces. Henry Chao, AIA, principal at HOK New York, recounts how his firm’s proposal (with Studio 505 and CPG) won the NTFGH competition by integrating the ground floor with nearby commercial buildings, pedestrian flow, and the Mass Rapid Transit system, so that NTFGH is a “hospital without walls,” seamlessly meshing with the urban fabric.
Most patient wards in Singapore, where healthcare is universal but stratified in a public/private system, are multi-bed, not single or double occupancy as in the U.S. With 82% of patient beds in passively cooled, naturally ventilated rooms, NTFGH’s floor plans stagger beds along sawtooth-shaped headwalls to give each patient a personal window, separating exhaled air and reducing pathogen transmission. (Diagnostic areas and treatment floors have air conditioning, which cools 30% of the hospital.)
Carnegie Mellon professor and EBD scholar Vivian Loftness, FAIA, notes that many interior features—green spaces and views, hands-free design minimizing surface transmission, and daylighting (including solar orientation and circadian color-temperature variation)—have strong research support. Natural ventilation, however, is “one of the big debates right now.” Despite American air-exchange codes and assumptions about bacteria, viruses, and pollutants, natural ventilation may actually improve air quality and reduce hospital-acquired infections. “We’re trying to strike an interesting balance here: how do we get the cleanest air possible under circumstances that support healing?” Baum says. “Studies indicate air-exchange rates are higher with natural ventilation with operable windows than with mechanical ventilation. But it’s less controllable, so that makes a lot of Americans nervous.”
“Mechanical systems are pretty badly maintained over time,” Loftness observes. “If you’re in an environment that isn’t highly polluted, nothing beats fresh air through an open window.” The proliferation of air-quality sensors, Baum adds, expedites monitoring of particulates, carbon monoxide, carbon dioxide, and other ventilation hazards. Designs need to accommodate metabolic and comfort differences between patients and staff. Loftness observes: “If all your thermal systems are geared toward nurses and doctors, the patients will be too cold,” with the converse leaving staff overheated. This underscores the value of individualized control.
Site variables are pivotal. Natural ventilation would be undesirable for a facility located near high levels of vehicular exhaust or plant allergens. Yet in most of the U.S., Roger suggests, it is feasible during temperate seasons. Considering the potential energy and cost savings, this long-established practice may make a comeback even in a nation accustomed to HVAC.



ROOM WITH A VIEW
American inpatient facilities are largely moving from double to single-bed rooms for both infection control and patient preference. Roger notes that retrofit projects must balance privacy, light, views, and safety concerns. “Typically, we want the toilet door to be as close to the patient as possible,” he notes, since “most falls occur as the patient leaves the bed to go to the toilet.” Simplifying that movement, providing sightlines to the corridor and the window, and minimizing isolation when an inboard bathroom blocks the corridor, he says, sometimes involves a hybrid room plan, “flipping the headwall” where gases and other utilities are located.
This can be expensive. “If you’re doing an entire unit of rooms,” Roger says, “you might simply be reversing the access to the gases in the wall for the next room over.” Studies have examined whether alternating or uniform-handed designs affect medical errors. In surgical and obstetrical areas, he says, “same-handedness is important, with everything in the same place because the same room is being utilized by multiple surgical teams.” In the patient room, however, “it hasn’t been proven beneficial. We think it is, but no one’s collected enough data to say it is definitively.” HOK estimated a cost increment around $1,200 per room for one hospital, he reports, which decided single-handed rooms were affordable.
Such cost-tradeoff decisions, Roger suggests, are best made on a long-range basis. His team studies the operational consequences of physical details—nurses’ travel distance between rooms, adjacencies, multifunctional spaces that can reduce footprint and construction costs—“but not skimping on things that increase safety, decrease problems, and make a happier staff,” he adds. Design, operations, and maintenance, he says, constitute “only about 8% of the 40-year life of a building.”
Loftness has linked EBD findings and the financial variables guiding owners’ decisions. Because ongoing personnel costs outweigh up-front costs, return-on-investment statistics for green amenities are persuasive. The savings may support features whose appeal awaits research confirmation, such as gardens or parks where patients can walk, as in Khoo Teck Puat (branded as “a hospital in a garden and a garden in a hospital”), or design contributions by acousticians, reducing noise so inpatients can sleep. “The notion that EBD is critical to the future,” she recognizes, “has not necessarily resulted in a concerted effort among architects, engineers, and the medical community, or federal funding to gather that data. But we’re getting the data from other countries.”



BRINGING CARE TO THE PATIENT
A recent trend is to extend healthcare to patients instead of drawing them to large centers. This distributive model operates on several scales. One involves internal practices like moving specialized equipment to a patient’s room rather than transporting the patient to an intensive-care unit. Waiting rooms are becoming obsolete as communication technology allows smoother remote triage. Yablon cites “patient-centered care” ambulatory facilities that eschew doctors’ offices entirely in favor of open collaborative spaces with separate entries for patients and physicians, saving patients from navigating corridors in exposed gowns for tests.
On the community level, Yablon has explored the satellite clinic. He has designed a series of renovated neighborhood public health centers first built under Mayor Fiorello LaGuardia: Mt. Sinai’s clinic in Manhattan’s Ansonia building, whose Beaux-Arts interior niches serve as work areas; and the Diane L. Max Health Center of Planned Parenthood in Long Island City, where color, daylight, and form are wayfinding aids for a polyglot Queens population and pastel-hued walls and graphics convey a sense of welcome.
Institutions’ outreach reflects an implicit power shift in contemporary healthcare. “The move will be to go even further, like being in shopping malls,” Yablon comments. “If your doctor’s running late, you can do something else; you’re not just stuck in a parking lot.” Competition for patients, he finds, drives revisions in operations and design, recognizing the value of patients’ time and perspectives.
Frances Halsband, FAIA, founding partner of Kliment Halsband Architects, identifies a key principle in her firm’s work with Mt. Sinai: “Somehow when you start talking about a patient, they stop being people—they become something else. In fact, what works for people works for patients. Patients are actually people—that’s the big revelation.”
New Mt. Sinai facilities, including a local plastic-surgery space and an ambulatory clinic in Kyabirwa, Uganda, extend patient-centric thinking to reinvention of spaces and processes, notes Halsband. She says that surgery chair Michael Marin, MD, who understands that design is critical in changing a hospital’s culture, “took me through his operating suite and said, ‘You see this enormous machine? We don’t need this. We just have it so we can bill Medicaid.’” The plastic-surgery suite eliminates excesses like waiting areas and cumbersome triage procedures in favor of roving concierges and large touch screens aiding doctor-patient communications. Kyabirwa’s clinic will save lives among the underserved through streamlined spaces appropriate to appendectomies, not technology meant for heart transplants.
“It’s not about innovation,” Halsband summarizes. “It’s about things we already know work well to make people feel comfortable in spaces they’re in. The challenge is to bring more of those things into an environment that’s become over-institutionalized.”
Aalto and Lubetkin would presumably approve.












